How Florida Medicaid Changes Will Impact ABA Providers
File this one under “Another change to keep up with.” Significant updates are coming to Florida Medicaid, and if you're an ABA provider, you’re probably wondering how this will affect your practice.
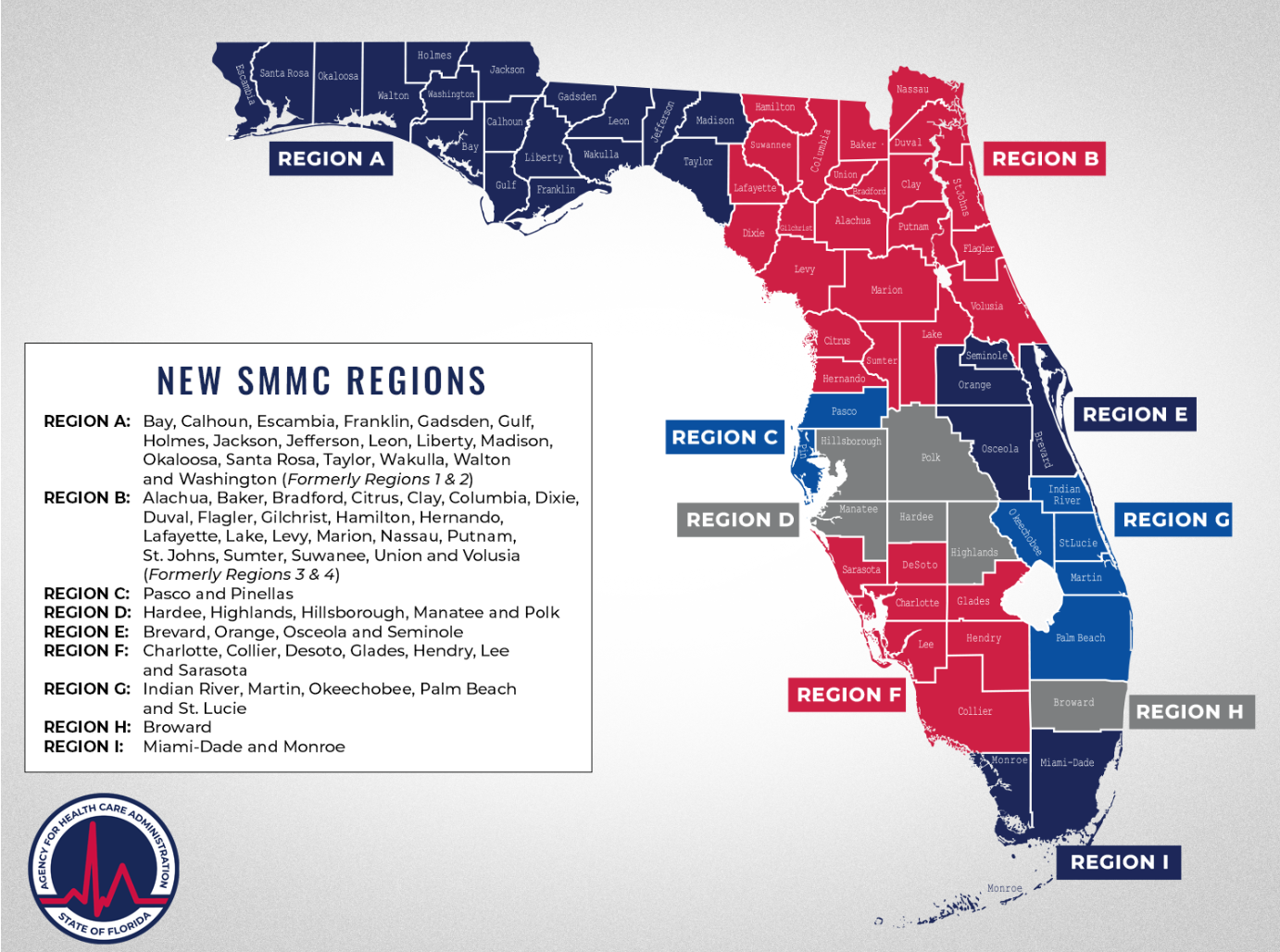
The Statewide Medicaid Managed Care (SMMC) program is restructuring, reducing Florida’s Medicaid regions from eleven to nine.
Click here to read the full details.
This change, set to take effect in February 2025, could have significant implications for ABA providers and the families they serve. While the number of Medicaid plans will remain the same, provider contracts, referral networks, and regional structures will be affected.
Basically, Senate Bill 1950 has realigned Florida’s counties, with the goal of improving efficiency in service delivery. However, the transition raises questions about potential disruptions in care, administrative burdens, and adjustments providers will need to make.
Now, you may be thinking, “Another change? I just got used to the current system!”
And if you’re like many ABA providers, you may even be a little uncertain about how this shift will impact your practice. Will this affect service continuity, credentialing, or contracting processes?
Here’s the breakdown of what it all means. Need more info, here is the direct link.
You Won’t Have to Navigate Eleven Different Regions Anymore
The previous Medicaid structure divided Florida into eleven separate regions, each with different health plans and referral networks. The transition to nine regions is intended to simplify service coordination, though it remains to be seen how it will affect access and administrative workload for providers.
You’ll Have to Adjust to a New Regional Map
The most immediate impact for providers is the need to familiarize themselves with the revised regional boundaries. If your practice operates in multiple regions, your Medicaid billing and authorization processes may require updates.Here’s a map to help you understand the new regional breakdown.
You May Need to Update Contracts and Referral Networks
Since Medicaid enrollees will still have multiple health plan options, providers must ensure their contracts align with the new regional boundaries. Some providers may find themselves needing to renegotiate agreements, which could create temporary administrative challenges.
Understanding the Florida Medicaid Behavior Analysis Services Coverage Policy
Who Can Receive Services
Florida Medicaid recipients under the age of 21 who require medically necessary behavior analysis (BA) services to address behaviors that impair their ability to perform major life activities. Such functional impairments include:
- Safety: Aggression, self-injury, property destruction, elopement
- Communication: Issues with expressive/receptive language, poor understanding or use of non-verbal communication, stereotyped or repetitive language
- Self-stimulating: Abnormal, inflexible, or intense preoccupations
- Self-care: Difficulty recognizing risks or danger, grooming, eating, or toileting
- Other: Complexity of treatment, programming, or environmental variables
Referral Requirements
The recipient must be referred by an independent physician or qualified practitioner who can assess and diagnose disorders related to functional impairment. Eligible referring providers include:
- Primary care physicians specializing in family practice, internal medicine, or pediatrics
- Board-certified or board-eligible physicians specializing in developmental behavioral pediatrics, neurodevelopmental pediatrics, pediatric neurology, adult or child psychiatry
- Licensed child psychologists
The updated Florida Medicaid Behavior Analysis Services Coverage Policy outlines new standards for behavior analysis services, including prior authorization requirements, documentation standards, and eligibility criteria. Providers should carefully review these changes to ensure compliance and avoid disruptions in reimbursement.
Key updates include:
- Revised guidelines for treatment plans and required documentation: Providers must ensure treatment plans include detailed measurable goals, parent training components, and documented progress to justify continued services.
- Adjustments to the supervision requirements for RBTs and other support staff: The new policy requires detailed compliance logs and documentation. Additionally, it outlines supervisor responsibilities for maintaining the integrity of treatment implementation.
- Specific criteria for the assessment and ongoing authorization of ABA services: Initial assessments must now include standardized assessment tools and data-driven justifications for ABA therapy. Ongoing authorization requires documented evidence of skill acquisition and a demonstrated need for continued therapy based on functional improvements.
While these updates aim to create consistency in service delivery, providers may experience an increased administrative burden in meeting the new documentation and authorization requirements.
Potential Impacts on ABA Services
While the stated goal of this transition is to create a more efficient Medicaid system, some providers are concerned about how these changes may impact service delivery and continuity of care. Providers should monitor updates closely to address any disruptions that could arise during the transition period.
As outlined in the Florida Medicaid Behavior Analysis Services Coverage Policy, these updates are expected to standardize administrative processes, though providers may face short-term challenges adjusting to new policies.
Key Takeaways
Florida Medicaid’s restructuring will affect ABA providers in multiple ways, and it’s crucial to prepare accordingly:
- Review the New Regions: Identify which region(s) your practice falls under and understand how this affects your services.
- Assess Provider Contracts: Check whether your agreements need to be updated to reflect new regional assignments.
- Understand Coverage Policy Updates: Ensure compliance with the revised Medicaid Behavior Analysis Services Coverage Policy to maintain proper authorization and reimbursement.
- Monitor for Additional Updates: Follow Florida Medicaid’s Behavior Analysis Services Information for ongoing developments.
Action Steps to Take Today
If you’re currently credentialed with Medicaid, begin reviewing your regional coverage and plan for potential administrative adjustments.
- Determine which new region(s) your practice falls under.
- Reach out to Medicaid contacts for clarification on contract modifications.
- Review the new coverage policy to ensure compliance with updated documentation and authorization requirements.
- Prepare your team for potential workflow changes as the transition approaches.
With careful preparation and ongoing monitoring, ABA providers can navigate these changes while continuing to provide essential services to their clients.
What’s your biggest concern about these changes? Share your thoughts in the comments!